Abstract

Background
A prior quality improvement (QI) initiative (Mikhael ASH 2020) was conducted to address root causes of racial disparities in care delivery among patients with relapsed/refractory (R/R) multiple myeloma (MM) in 2 large oncology systems. Preliminary survey data suggested discordant beliefs regarding patients’ primary treatment concerns. Thus, this study was scaled up to 4 community-based oncology practices to greater evaluate disparities with electronic medical record (EMR) audits and team-based audit-feedback (AF) sessions to identify factors which could enhance more equitable care.
Methods
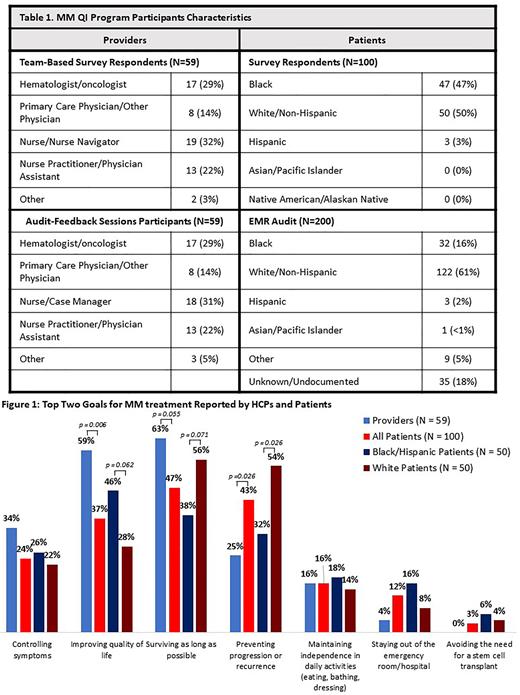
This QI initiative included patient and provider surveys, baseline and follow-up EMR audits, and small-group, team-based AF sessions at each participating clinic. Surveys were completed by 59 hematology/oncology healthcare providers (HCPs) and 100 R/R MM patients (Table 1; N=47 Black, N=50 White/Non-Hispanic) to examine alignments and discordances in attitudes, beliefs, perceptions, and practices regarding MM care. A baseline EMR audit of 200 R/R MM patients (Table 1; N=32 Black, N=122 White/Non-Hispanic) was conducted to identify patient/disease characteristics, treatment history, clinical practice metrics, and patient-centered measures (e.g., shared decision-making). During 1-hour AF sessions, HCP cohorts (Table 1) (a) assessed clinic-specific practice gaps identified by the patient-provider surveys and baseline EMR audit, (b) prioritized areas for improvement, and (c) developed action plans to address root causes. Surveys completed before (N=59) and after (N=41) the AF sessions measured changes in participants’ beliefs and confidence in care delivery. A follow-up EMR audit after completion of the AF sessions was performed to assess behavioral and practice change.
Results
Patient and HCP tethered survey data revealed discordant beliefs about patients’ primary treatment concerns. HCPs overestimated patients concern regarding treatment cost (32% vs 9%) and treatmentrisks (55% vs 29%), but underestimated patient's largest reported challenge in feeling confident that their treatment plan is the best for their cancer (18% vs 32%). Providers reported the most challenging aspect of MM management was individualizing treatment plans.
There was large divergence between HCPs and all patients’ top goals (Figure 1) and stark racial disparities were observed in improving quality of life, preventing progression or recurrence, and surviving as long as possible (Figure 1). Disparities also persisted among patients who reported being on track or somewhat on track to achieve their treatment goals (76% White vs 54% Black/Hispanic, p = 0.021). Regarding shared decision-making (SDM) with their HCP, only 14% of Black/Hispanic patients felt completely involved in treatment decision making compared to 54% of White patients (p = < 0.001). EMR audits revealed fewer Black patients using maintenance therapy (63% vs 71% non-Black) and greater numbers of stem cell transplants (53% Black vs 44% non-Black).
Following AF sessions 55% of HCPs set action plans to incorporate strategies to eliminate disparities in care for diverse MM patient populations and 48% to develop personalized treatment plans incorporating patient-specific factors and preferences. To achieve these goals, providers committed to engage patients in shared decision-making (17% pre-AF vs 38% post-AF), and provide adequate patient education about treatments (17% pre-AF vs 28% post-AF). Participants’ views of the impact of race and socioeconomic factors on equitable MM care changed as a result of the program increasing from 37% to 54% reporting a considerable or a great deal of impact.
Conclusions
Barriers to equitable, patient-centered care in patients with R/R MM included inadequate education and personalizing of treatment plans by HCPs as well as ineffective SDM. Discordances were observed between providers and all patients in describing the goals of treatment, and between White and Black/Hispanic patients in the challenges faced in their MM care. Action plans developed during this QI initiative intend to address identified gaps and improve equitable care for patients with R/R MM.
Study Sponsor Statement
The study reported in this abstract was funded by independent educational grants from AbbVie, Inc. Bristol-Myers Squibb, and Janssen Biotech Inc., who had no role in the study design, execution, analysis, or reporting.
Disclosures
Mikhael:Amgen: Consultancy; Sanofi: Consultancy; GlaxoSmithKline: Consultancy; Janssen: Consultancy; Karyopharm Therapeutics: Consultancy; BMS: Consultancy; Takeda: Consultancy.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal